Cardiology Check Up
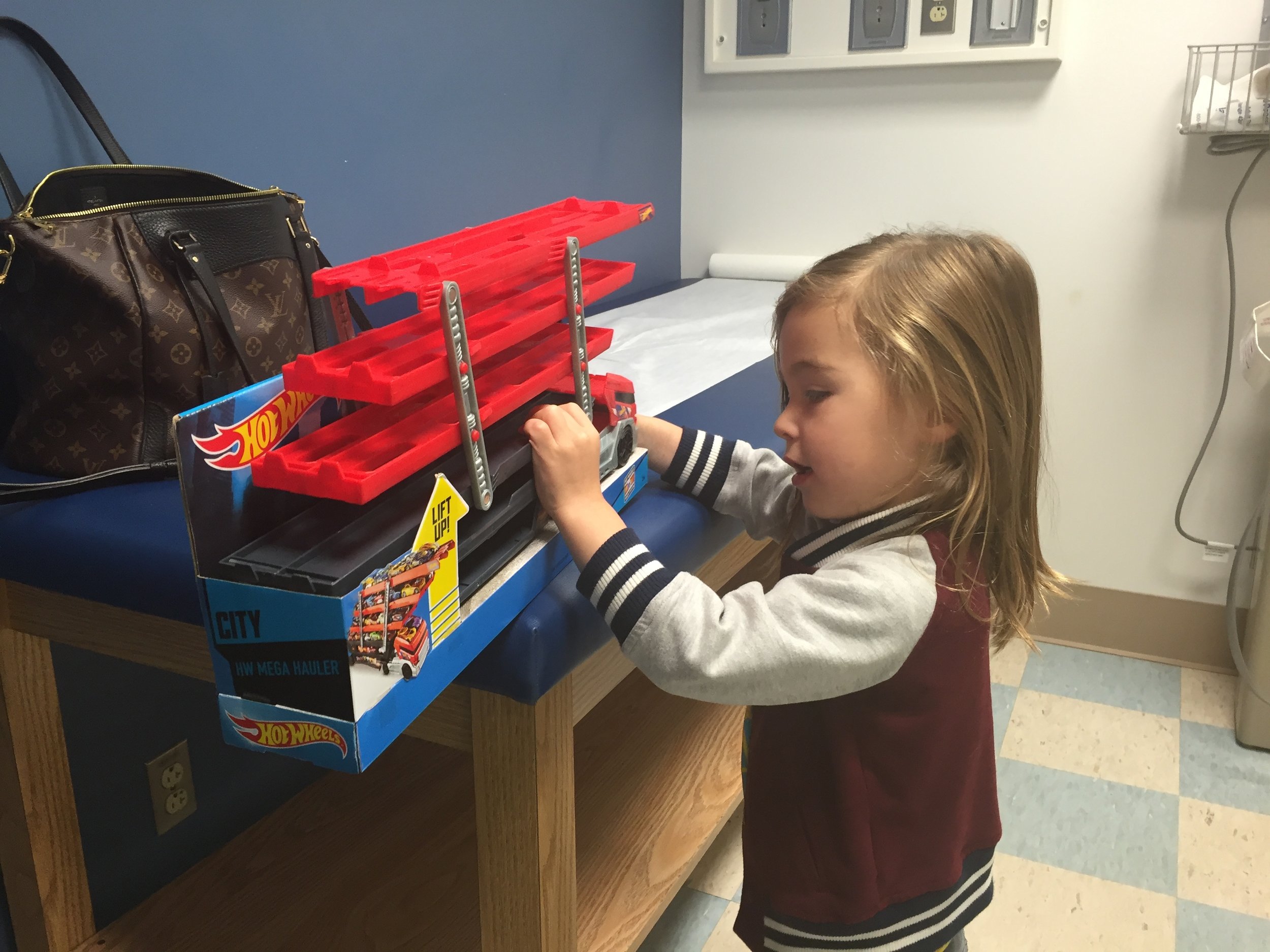
/It's hard to believe it has been 1 year since Santi had the Fontan, his third open heart surgery. Santi has recovered beautifully from his surgery and his heart function is excellent. Words every heart family longs to hear. We are down to annual cardiology visits, which is also phenomenal for a young HLHSer. Santi's highlight to our (4 hour!) appointment, was getting this cool Hot Wheels car carrier. It certainly helped us get through the last hour of waiting around. We were sent home in a Holter Monitor (24 hour EKG) which is pretty standard. Santi will wear it for a day, then I mail it back to the doctor and they read his heart rhythms. My little trooper did great today and we are happy to hear his heart is doing well!
November 2014
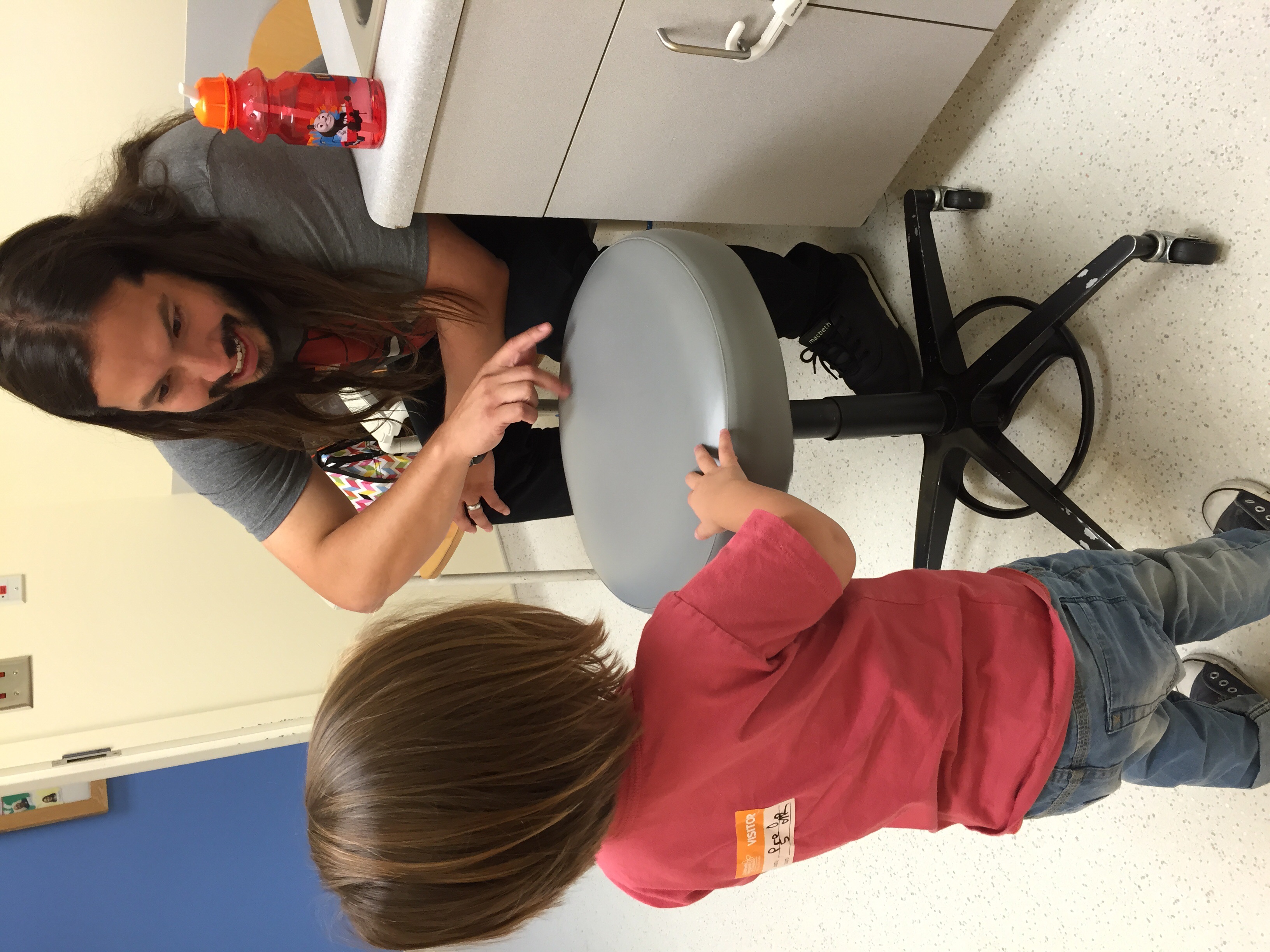
One year ago, Santiago recovering from the Fontan